Blood glucose monitoring and Insulin pumps
Checking your blood glucose (BG) readings regularly – and responding to the readings – are the two most important things that people can do to ensure their success and safety with insulin pump therapy.
When people start on pump therapy, they’re usually taught by their health care team to check their BG quite frequently. In fact, for the first couple of weeks, it’s wise to check it eight to ten times per day. This includes:
- Before each meal (breakfast, lunch, and dinner) and two hours after each meal: comparing your pre-meal BG level to your post-meal BG level allows you to determine if your insulin-to-carbohydrate ratio is set correctly.
- Bedtime, every three to four hours during sleep, and when you first wake up in the morning: comparing your BG level during your sleep schedule allows you to determine if your overnight basal rates are set correctly.
These readings will provide you and your health care team with the information needed to adjust the settings on your pump so that they can be fine-tuned specifically for you. Some of the settings that may need to be adjusted include your basal rate, insulin-to-carbohydrate ratio, correction factor and target ranges.
Once you learn how to use the pump – and the settings are adjusted correctly – you can have better BG control.
After the initial two-week period of checking, you should check your BG four to six times each day. The table below shows when people who are routinely using pump therapy should check their BG, and why.
| Check BG | Why? |
| When you first wake up | Shows if fasting BGs are high or low |
| Before each meal (breakfast, lunch, and dinner) |
Determines if you need to take additional insulin for a BG that is above your target or less insulin if your BG is below your target range |
| Bedtime | Provides information to help you make adjustments to prevent low or high BGs during sleep |
| Occasionally during the night (at 3:00 am) |
Allows you to see if your BG levels are stable through the night and if your nighttime basal rates are set correctly |
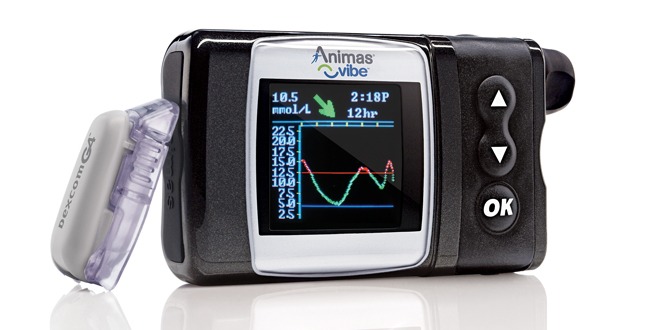
Continuous glucose monitoring (CGM) and insulin pumps
A CGM system can be used when you wear a pump for insulin delivery, or without pump therapy as a standalone. Many pump users find CGM quite helpful in their overall diabetes management. CGM isn't the same as BG monitoring, as sensors are placed into your body and transmit BG results to a pump or CGM receiver. The sensors measure the glucose in your interstitial fluid (the fluid in and around your body’s cells).
A CGM system senses and records glucose levels every five minutes, which means it can show trends, i.e. whether BG levels are rising or falling. In contrast, blood glucose meters provide you with only a “snapshot” of your BG levels at a particular point in time. Thus, a CGM system can show users their glucose trends as they develop and help them to make more timely changes.
The Canadian Diabetes Association’s recent clinical practice guidelines note that recent advances in CGM systems may augment the diabetes management of people who use an insulin pump.
Furthermore, it has been shown in studies that pump therapy and CGM systems, when used together, result in fewer episodes of hypoglycemia than with traditional BG testing. In fact, a recent study was conducted on 485 people with type 1 diabetes, who were not well-controlled in their diabetes management. The study participants were split into two groups: those who were using pump therapy and a CGM system, and those who used multiple daily insulin injections of insulin to manage their type 1 diabetes. At the end of the study, the participants who used an insulin pump plus a CGM system to manage their diabetes had significantly lower A1C and BG levels.
CGM is recommended for people with diabetes who are willing and able to use it properly, and can calibrate it as needed. It is especially recommended for people who:
- Suffer from frequent episodes of hypoglycemia, which cause problems with daily activities
- Have an extreme fear of hypoglycemia
- Suffer from episodes of severe hypoglycemia – despite optimized use of insulin therapy and conventional BG monitoring
- Have hypoglycemia unawareness
This article was sponsored by an unrestricted educational grant from Animas Canada.
 Diabetes Care Community Learn, connect and care
Diabetes Care Community Learn, connect and care