Individuals who are newly diagnosed with type 2 diabetes can expect to be placed on medications much more quickly than in the past.
This is due to an important change in the latest Clinical Practice Guidelines, released in April 2013. Under the old guidelines, the goal was to help patients reach A1C targets within 6 – 12 months. However the new Guidelines recommend that this goal should be achieved at a much earlier stage. That is, within 3 – 6 months of diagnosis.
This means there is much less ‘waiting around’ to see if lifestyle management can bring blood glucose levels back to normal. In short, if lifestyle changes are unable to stabilize blood glucose levels within 2 – 3 months after diagnosis, medications will be prescribed.
The initial medication of choice for type 2 diabetes is usually metformin. Often, more than one medication will be recommended. For some people, the additional medication will be insulin.
What is an A1C?
The A1C lab test shows your average blood glucose levels over the past two or three months. The test does not require fasting, and has recently been used as one of the tests for diagnosis of diabetes or prediabetes.
The A1C test is also one of the most important tools for ongoing diabetes management, which is based on keeping blood glucose levels within normal targets. By monitoring blood glucose levels over time, the A1C test can help healthcare professionals identify when medications or lifestyle habits need adjusting. This helps to reduce the risk of diabetes complications.
What are normal A1C targets?
A1C for diagnosing diabetes:
The 2013 Clinical Practice Guidelines state that a diagnosis of diabetes may be made when the A1C result is over 6.5%. An A1C of between 6.0% to 6.4% may result in a diagnosis of prediabetes.
A1C targets for people living with diabetes:
It is recommended that most people with diabetes achieve an A1C target of below 7.0% within 3-6 months of diagnosis. Every person’s target range is individualized, so make sure you discuss your target range with your doctor. There may be reasons why your A1C target range is higher or lower than 7.0%.
If the A1C reports blood glucose levels of over 7% 3-6 months after diagnosis, medication will be prescribed. When levels exceed 8.5%, a combination of two medications may be recommended.
How often should you have an A1C test?
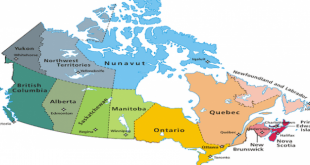
The recommendation from the Canadian Diabetes Association is for an A1C test every three months. Frequency of testing may be reduced to once every six months if blood glucose levels appear to have dropped into the normal range.
What can you do to improve A1C levels?
If you are newly diagnosed with diabetes, you can work towards your A1C targets by making lifestyle changes. Healthy eating and regular physical activity can play an important role in reducing blood glucose levels. Reaching and maintaining a healthy weight can also make a significant impact on A1C results, and can help reduce the risk of diabetes complications.
Will you be stuck on drugs like metformin for life?
The answer depends upon individual health and blood glucose levels, and upon an individual’s ability to make lifestyle changes. You may find it helpful to read our article on this site entitled Tips for weaning off medications for type 2 diabetes.
As we have discussed, diabetes management is based on maintaining blood glucose levels within normal ranges. This generally requires the use of medications such as metformin.
However, if an individual shows they can maintain healthy blood glucose levels entirely through weight maintenance and a healthy lifestyle program, metformin may be discontinued under a healthcare professional’s direction.
Keep in mind that even if you are able to manage successfully without medications at any point in time, you will still have diabetes. This means you may need to return to a medication schedule in the future.
For more information, check out our expert’s blog Oral medications for type 2 diabetes – do I have to? And also check out our video Type 2 Diabetes Medications – Reach Your Goals.
 Diabetes Care Community Learn, connect and care
Diabetes Care Community Learn, connect and care