
Do you have a child with Type 1 Diabetes?
You are not alone.
Many children in Canada inject to manage their diabetes. Injecting isn't difficult. It's easy to learn. It's quick and more comfortable than you would think. Your approach with your child, will greatly affect how quickly he adjusts. If you are anxious and frightened about giving your child a needle he will also be anxious and frightened.

There are a number of creative things you can do to help with your child’s daily injection routine.
- Prepare the injection out of sight.
- Approach your child in a matter-of fact manner, stating that it is time for “insulin". Do not use the word “needle”.
- Offer a simple explanation as to why she needs insulin. For example: to help you grow and be strong.
- Tell your child that sometimes insulin hurts and it is okay for him to cry, but his job is to stay still.
- Avoid negotiating and bribing and deliver the injection quickly.
- Restrain your child if necessary.
- Give your child a hug and kiss after the injection is over.
How should I give the insulin injection?
Tips for toddlers, preschoolers and early school-aged children:
- Try to keep your child distracted while giving the injection. For example: watching T.V., playing with your phone, wiggling toes, counting, blowing bubbles or finding objects in a picture.
- Let your child help prepare the injection. For example: mixing the cloudy insulin, screwing on the pen needle, and doing the 2 unit “air shot” with the insulin pen.
- Pretend that one of their stuffed animals or dolls has diabetes and let her give it injections with a syringe that has the needle cut off or an insulin pen without a pen needle attached.
- Use a sticker chart to encourage your child to hold still for injections. After he has earned a certain number of stickers you might want to offer a small reward such as a coin or a pack of sugar free gum.

Note: give a reward for 3-5 stickers for a 3 year old and 5-8 for a 5 year old.
Did you know?
Structured site rotation is critical for protecting your child’s injection sites.
Small children do not have much surface area at injection sites. If injections are given in limited spots, fatty lumps may form. These lumps are called lipohypertrophies. Lipohypertrophy can become unsightly looking and insulin is poorly absorbed from them.
To prevent lipohypertrophy:
- Inspect and feel your child’s injection sites on a regular basis and ensure that your doctor or diabetes educator does so at each visit.
- Ask your doctor or diabetes educator to help you identify other potential injection sites.
- If your child is anxious about trying new sites, consider using a sticker chart when a new site is used and offering a bravery award after a certain number of stickers are earned.
- Most importantly, do not let your child “call the shots” on where insulin is to be given!
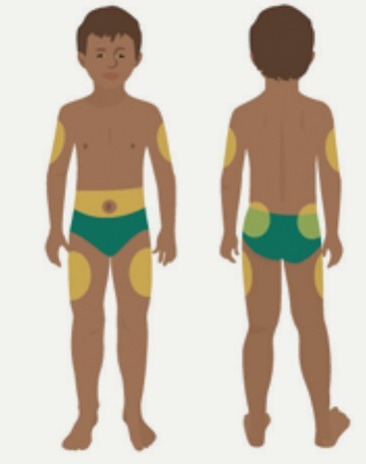
Up, Down and All Around Chart?

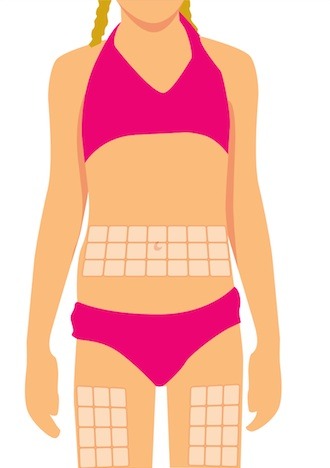

Ideas for Use:
- Reward your child with a sticker for holding still for an injection.
- Put an "X" through any lipohypertrophies (lumps).
- Place stickers on new sites when they are used.
- Reward "bravery" stickers for trying new injection sites.
1 Lo Presti D, et al. Skin and subcutaneous thickness at injecting sites in children with diabetes: ultrasound findings and recommendations for giving injection. Pediatric Diabetes 2012; 13(7): 525-33 2 Howe CJ, Ratcliff, SJ, Tuttle A, Dougherty S, Lippman TH. Needle anxiety in children with type 1 diabetes and their mothers. Maternal Child Nursing 2011; Jan/Feb: 25-31. 3 Patton SR, Eder S, Schwab J, Sisson CM. Survey of insulin site rotation in youth with type 1 diabetes. Journal of Pediatric Health Care 2010; 24, 365-371. 4 Berard L, et al. FIT Forum for Injection Technique Canada. Recommendations for Best Practice in Injection Technique. October 2011.
Supported by BD Medical – Diabetes Care
11-2013
 Diabetes Care Community Learn, connect and care
Diabetes Care Community Learn, connect and care




